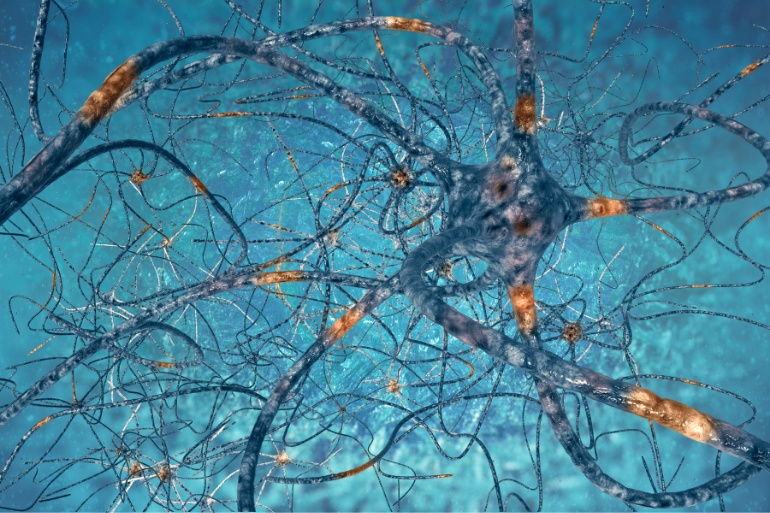
Neurodegenerative Diseases is a broad term that includes various diseases of the nervous system. The brain and spinal cord are the organs of the nervous system, which, in turn, is made up of billions of cells, the neurons.
As a rule, the reproduction and renewal of neurons is not possible. Therefore, in case of damage or apoptosis, it is impossible for them to be replaced.
Neurodegenerative Diseases are caused as a result of primary degeneration of neurons of the nervous system in specific anatomical areas of the brain. In particular, the structure and function of neurons in distinct areas of the nervous system are disrupted and specific cell populations are affected.
The most common Neurodegenerative Diseases include Alzheimer’s Disease (AD) and other forms of Dementia, Parkinson’s Disease (PD) and Parkinson’s Disease-related disorders, Multiple Sclerosis, Motor Neurone Disease (MND), Myasthenia Gravis, Huntington’s Disease (HD), Spinal Cord Ataxia (SCA), Spinal Muscular Atrophy (SMA) and Myotrophic Lateral Sclerosis.
The Epidemiology of Neurodegenerative Diseases
These diseases mainly affect the elderly. Due to improved life expectancy, there is an increase in Neurodegenerative Diseases. These diseases can also affect people aged 30 to 40 years. This is of course a rare phenomenon and is usually due to aggravating genetic or environmental factors.
The pathophysiology and effects of Neurodegenerative Diseases
What characterizes Neurodegenerative Diseases is the misfolding of proteins, which accumulate, leading to the development of endoneuronic inclusions or plaques. Proteins that exhibit folding disorders are considered “toxic” and cause neuronal degeneration.
Neurodegenerative Diseases cause adverse effects on the quality of life of patients. Progressive degeneration and / or apoptosis of nerve cells implies problems in movement and mental function.
Gradually, dysfunctions are caused in multiple higher mental functions (memory, speech, orientation, critical ability, executive abilities, etc.). Furthermore, deregulations arise in the emotion, behavior, mobility and in general in the overall functionality of the patients, who cease to be autonomous and begin to depend on those around them. The quality of life of both patients and their families is significantly degraded.
The Contribution of Precision Medicine to the Therapeutic Approach to Neurodegenerative Diseases
Precision Medicine is the most modern Medical Approach, which aims at the prevention and detailed detection of the mechanisms of Neurodegenerative Diseases, at cellular and genetic level. To achieve these goals, it relies on certain pillars.
Performing Precision Tests
Through Specialized Tests at a Molecular and Genetic level, the causes of deviation of biochemical imbalances are identified and the springboard for the prognosis and diagnosis of Neurodegenerative Diseases is provided. Molecular Tests detect the metabolic profile of the organism under test with complete accuracy, while, with the help of Gene Tests, 1028 polymorphisms (SNPs), 507 genes and 62 diseases, which may be related to Neurodegenerative Diseases, are assessed.
This precise diagnostic approach assists in deciphering the predisposition of individuals to develop Neurodegenerative Diseases and identifies the implicated molecular and biochemical mechanisms in case the disease has already been expressed.
With these methods, even if genes are predisposed to the development of a Neurodegenerative Disease, certain lifestyle factors can help modify the expression of genes and thus suppress and / or neutralize the mechanisms that lead to inflammation and degeneration.
Personalized Therapeutic Schemes
Based on accurate analyzes, complete epigenetic history, the existence of underlying diseases, sex, age of the patient and many additional factors, an Interdisciplinary Team, composed of Physicians, Geneticists, Molecular Biologists, Biochemists and Molecular Nutritionists, can now formulate, for each patient, an individualized treatment regimen.
These Therapeutic Protocols assist in the treatment of Neurodegenerative Diseases, based on the application of antioxidants, anti-inflammatory and protective vascular or other biological mechanisms and not solely on chemical medication.
In clinical practice, they have been used since 1997 in the United States of America and in most cases there is not a contraindication with any other therapeutic scheme (e.g. homeopathetic drugs). The average duration of treatment for Neurodegenerative Diseases, depending on the patient’s clinical condition, can last from six to twenty-four months.
The results of such treatments are promising, with gradual restoration of the respective Morbidity. Patients who follow this type of treatment gradually see their daily lives improve, along with their overall physical condition. Their quality of life is promoted, their body is regulated, their mental and physical reserves are strengthened and any chances of recurrence of the disease are minimized. Thus, the therapeutic benefit of the patients is maximized and at the same time the unnecessary expenses are reduced.
References:
- Erkkinen, Michael G.; Kim, Mee-Ohk; Geschwind, Michael D (April 2018). “Clinical Neurology and Epidemiology of the Major Neurodegenerative Diseases”. Cold Spring Harbor Perspectives in Biology. 10 (4): 20. doi:10.1101/cshperspect.a033118. PMC 5880171.
- Stephenson, J.; Nutma, E.; van der Valk, P.; Amor, S. Inflammation in CNS neurodegenerative diseases. Immunology 2018, 154, 204–219.
- “What is Neurodegenerative Disease?”. JPND Research. JPND Research. 17 July 2014. Retrieved February 7, 2015.
- Maynard S, Fang EF, Scheibye-Knudsen M, Croteau DL, Bohr VA (September 2015). “DNA Damage, DNA Repair, Aging, and Neurodegeneration”. Cold Spring Harbor Perspectives in Medicine. 5 (10): a025130. doi:10.1101/cshperspect.a025130. PMC 4588127. PMID 26385091.
- Chung, CG; Lee, H; Lee, SB (September 2018). “Mechanisms of protein toxicity in neurodegenerative diseases”. Cellular and Molecular Life Sciences. 75 (17): 3159–3180. doi:10.1007/s00018-018-2854-4. PMC 6063327. PMID 29947927.
- Wang H, Dharmalingam P, Vasquez V, Mitra J, Boldogh I, Rao KS, et al. (January 2017). “Chronic oxidative damage together with genome repair deficiency in the neurons is a double whammy for neurodegeneration: Is damage response signaling a potential therapeutic target?”. Mechanisms of Ageing and Development. 161 (Pt A): 163–176. doi:10.1016/j.mad.2016.09.005. PMC 5316312. PMID 27663141.
- Lu YF, Goldstein DB, Angrist M, Cavalleri G (July 2014). “Personalized medicine and human genetic diversity”. Cold Spring Harbor Perspectives in Medicine (Essay). 4 (9): a008581. doi:10.1101/cshperspect.a008581. PMC 4143101. PMID 25059740.
- Ashley EA (August 2016). “Towards precision medicine”. Nature Reviews. Genetics. 17 (9): 507–22. doi:10.1038/nrg.2016.86. PMID 27528417. S2CID 2609065.